Why We Use Titanium Mesh Among Other Surgical Materials
In several FFS procedures, plates, screws, mesh and/or sutures of distinct types and materials are employed. This article aims to explain why each is selected as best for certain surgeries, as well as the pros and cons of each material.
Characteristics of surgical materials
Currently there are different types of materials for bone fixation, developed alongside many specialties, such as traumatology. Technological advances will likely generate a revolution in the field of biocompatible materials that we will surely begin to use in the future.
Many of you ask why we do not use resorbable materials. The reasons lay in the scientific literature, which does not solidly support the use of resorbable material as an alternative to the effectiveness of titanium in the adult population.
Below we’ll delve into the nature of surgical materials employed in FFS Surgery.
Titanium Material
Titanium is the material of excellence in maxillofacial procedures, as well as in numerous medical disciplines.
To date, the scientific literature favoring titanium material in facial traumatology, craniofacial surgery and facial feminization is overwhelming.
It continues to be the material of choice, being routinely tested in new formats by experts all over the world.
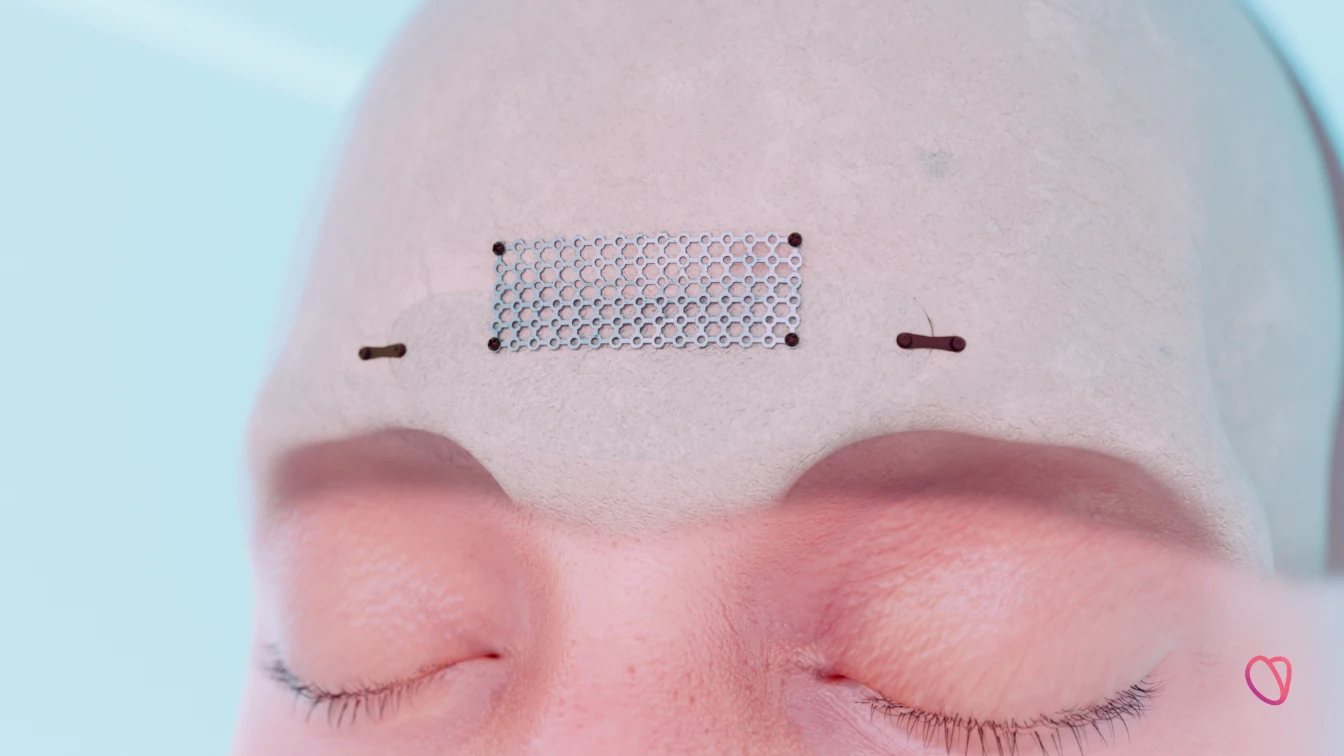
Our pioneering FOREContour® procedure technology, exemplified in the accompanying 3D video, showcases the ingenious utilization of titanium mesh.
This video not only offers a visual insight into the intricacies of the procedure but also underscores the indispensable role that titanium plays in achieving optimal outcomes
In conclusion, while titanium undeniably stands as the material of excellence in various medical disciplines, a nuanced evaluation of its pros and cons remains imperative for informed decision-making in the ever-evolving landscape of medical advancements.
So what are the pros and cons of the use of titanium materials?
Pros of Medical-grade Titanium
- Safety: The “urban legends” that have been generated about titanium are purely anecdotal. For the last 70 years, people with titanium materials have safely crossed airport security scanners and undergone all types of x-rays (just inform the radiologist in order to detect “artifacts” or alterations in images as a result). Millions of people safely live with dental implants, knee parts and hip prosthetics made of titanium on the planet today.
- Biocompatibility: To date, titanium is one of the best-accepted materials by the human body. Since the 1950s, hardly any case histories of rejection or intolerance to medical grade titanium have arisen.
- Favors bone regrowth: We know from our own experience that the use of certain titanium material (especially mesh) favors the generation of new bone below its surface, which further increases bone integrity in the mid and long term.
- Strength and Stability: Titanium material is highly durable and capable of immediate “load-bearing” stability for bone fragments. It’s resistant to changes in shape and structure over time, which is especially important for complex fractures or reconstructions.
- Flexible Applications: Titanium mesh can be easily bent and shaped intraoperatively designed to match the desired contour.
- Long-lasting: Titanium is a non-corrosive material that does not degrade or break down over time, ensuring a long-lasting solution for structural support.
- Radiopacity: Titanium is radiopaque, meaning it can be easily visualized on imaging techniques like X-rays, CT scans, and MRIs. This aids in post-operative assessments as it is not an impediment to having radiodiagnostics.
Cons of Medical-grade Titanium
- Metal Sensitivity: Some patients may have allergies or sensitivities to metals like titanium, which can lead to discomfort or complications. The percentage of this type of reaction is statistically insignificant.
- Risk of Infection: The presence of a non-resorbable material like titanium mesh can potentially increase the risk of infection if proper aseptic techniques are not followed during implantation.
- Invasive Removal: If it is necessary to remove the titanium material, a new intervention will be required, which may entail additional risks and costs. The reasons that make it necessary to remove the titanium material are varied and can range from infection, resorption of the peripheral bone, irritation of a nearby nerve branch or the fact that the material may be palpable or visible on certain occasions. In our experience to date, the incidence of titanium mesh removal is less than 2% of the total meshes placed–again indicating the relative reliability of titanium mesh.
Resorbable Material
This is the material of choice in pediatric craniofacial surgery due to the fact they are growing, hence the need for the material to disappear promptly in order to avoid the issues of migration (displacement) during the developmental phases. To date, the most frequently used component is polylactic acid or its derivatives.
However, there is no scientific or medical evidence that supports the use of resorbable material in facial feminization surgery.
Let’s review some pros and cons of resorbable material:
Pros of Resorbable Material
- Biocompatibility: Resorbable mesh materials are designed to be compatible with the body’s tissues, reducing the risk of adverse reactions or sensitivities.
- No Need for Removal: One of the main advantages of resorbable mesh is that it gradually degrades over time and is eventually absorbed by the body. This reduces the need for a second surgical procedure for removal if deemed necessary.
- Reduced Infection Risk: The temporary nature of resorbable mesh can potentially reduce the risk of infection compared to a permanent material like titanium.
- Gradual Load Transfer: Resorbable mesh gradually transfers load to the healing bone, which can be advantageous in certain cases to promote natural bone remodeling.
Cons of Resorbable Material
- Limited Strength: Resorbable mesh is generally not as strong as titanium mesh, making it less suitable for complex fractures or areas requiring substantial structural support such as the Forehead reconstruction. In the cases where bone defects appear after the frontal setback, it is mandatory to cover them with a permanent, rigid mesh, so resorbable mesh is not recommended.
- Variable Resorption Rate: The rate at which resorbable mesh degrades can vary among patients and even within the same patient, potentially leading to unpredictable outcomes. There are even some cases where the material remains intact after 12-15 months.
- Radiolucency: Resorbable mesh is often radiolucent, which means it is not easily visible on imaging, making postoperative evaluation more challenging.
- Slow Load-Bearing: Due to its gradual degradation, resorbable mesh may not be able to bear loads immediately, necessitating a period of restricted function.
- Inflammation: The skin of the frontal region is very thin. The installation of a material such as polylactic acid generates an inflammatory reaction (necessary for the degradation of the material itself) that could be evident in the area where it is placed, generating a visible aesthetic defect during the time it takes to dissolve (from 3 months to 5 years). A priori it could be a significant handicap for feminization patients.
Other Materials
Stainless steel material
The use of stainless steel in the form of steel threads is extremely limited and with hardly any scientific support in adult facial and craniofacial feminization surgery. However, some specialists use it as an anchoring and fixing material due to its much lower cost than titanium material. Today there is no reconstruction material itself (plates, screws, meshes…) made of stainless steel.
Bone paste
Bone paste, also known as bone cement or bone filler, is a medical substance that is commonly used in orthopedic surgery to fill voids or gaps in bone tissue.
It is typically made from a mixture of polymethylmethacrylate (PMMA) powder and a liquid monomer, which, when combined, form a paste-like material that hardens rapidly. This substance has been widely used in various orthopedic procedures, most notably in joint replacement surgeries like hip and knee replacements.
Bone paste is employed for several purposes:
- Fixation in Joint Replacement: In joint replacement surgeries, bone paste is often used to secure implants like prosthetic joints to the existing bone. It helps to provide stability and promote the integration of the implant with the natural bone.
- Filling Voids and Fractures: Bone paste is used to fill voids or gaps that may be present due to bone loss, fractures, or other structural issues. It can provide structural support and stability to weakened bones.
- Augmentation: In certain cases, bone paste is used to augment or enhance bone structure. This can be done to improve the fit of an implant or to provide additional support to compromised bone.
Some surgeons use cement as a material to round the shape of the forehead, adding volume to the frontal bossing. The intention is to camouflage the excess bone in the supraorbital region. However, this goes against feminization surgery itself. As we well know, the objective of facial feminization is to eliminate the excess bone volume generated by testosterone during puberty. Adding volume results in an increase in the size of the forehead, contrary to the principles of our surgery. In addition to this conceptual problem, using excess bone cement has some added problems.
Note: As an alternative, for small fillers, we have bone powder from the patient’s own bone, shaved during the forehead remodeling surgery, which is in the same surgical field and at the same time, representing a useful alternative tool to use of foreign materials. This type of filling does not in any case replace the osteosynthesis material necessary for adequate fixation of areas where there is some bone discontinuity. It is a material that is obtained in a clean and simple way during surgery, which allows its easy application, especially useful for covering areas where the medullary bone has been exposed or areas with small gaps or excessively thin.
Why Facialteam prefers titanium fixation material

It’s essential for the surgical team to carefully consider these pros and cons to make an informed decision that will result in the best possible outcome for the patient.
Frontal feminization surgery involves the reconstruction of the frontal sinus in 95% of cases, a complex anatomical remodeling that must sustain the functionality of the frontal sinus as well as preserve the structural integrity of this facial region. For these and many other reasons, titanium is undoubtedly our material of choice.
The limited scientific support and the absence of a large series of patients reconstructed with resorbable material mean that for us it does not work as the material of choice.
Only in very selected cases can we choose to use it, such as in those patients with a clear allergy/intolerance to titanium, as long as the case meets the appropriate medical criteria and they accept the consequences of its use and the potential outcomes.
The future of surgical materials on the horizon
We hope that soon, tissue bioengineering will make it possible to generate biocompatible structures in the laboratory from cells from each patient, which can be cultured in the laboratory and pre-formed according to the need obtained during the virtual planning of each case.
Today it is already possible to manufacture them in vitro, just waiting for biocompatibility and behavior studies over time in real patients.
In addition, work is being done on another type of non-metallic material, with mineral characteristics, that can be designed and printed in 3D, which, once placed, allows the individual’s cells to regenerate and cover the defect, with the material disappearing once this function has been fulfilled. It is in the initial stages and it is possible that in a matter of 2-3 years this material will be available for use in surgery.
Takeaway message
After more than 15 years in the discipline, we know that forehead feminization is a proven, safe, reproducible and predictable procedure. Among the possible fixation materials, titanium is one of those that offers the greatest advantages and the one that has the greatest range and scientific support.
Many of you have broken bones in your body or had other surgery and know that afterwards, it is inevitable that healing may involve degrees of stiffness, tightness, swelling and numbness. Whether we like to admit it or not, there are consequences when our bodies are modified, be it changes in sensitivity, strength, scarring or symmetry.
Despite the fact that a pre-planned procedure has the advantage of foresight to minimize these consequences during the surgery or in the bone healing phases– differences may remain. This is to be expected in any maxillofacial surgery as bones are shaved, filed and/or deliberately fractured, although under the most controlled and safe circumstances.
Finally, read our blog about potential Healing anomalies, their prevention and solutions for a realistic point-of-view on FFS surgery expectations. Below you may find our replies to many FAQ’s from the community on the topic of titanium materials.
FAQ’s about implanted surgical materials
When is the titanium mesh necessary?
The mesh is necessary to strengthen those bone regions that have been weakened after frontal feminization surgery or to cover defects in the anterior wall of the frontal sinus.
If my skull bone is thick, why use a titanium fixation material?
Titanium is necessary as a material to fix the osteotomy of the anterior wall. Although it is true that it is not necessary in all cases, 95% of patients require reconstruction of the anterior wall (osteotomy + fixation with osteosynthesis material). This is true even in solid breasts (without air inside), since shaving could cause exposure of the medullary bone, much more prone to the phenomenon of resorption in the future. Furthermore, it would be more difficult to control the location of the posterior wall of the sinus, which could lead to larger complications.
Once healed, is the mesh still really needed?
Normally we could say no, but removing this material would imply a “big” surgery, so it is preferable to leave it in place, unless it implies some problem for the patient. What we know for sure is that the mesh, if it has been used, is absolutely necessary during the healing and bone regeneration phases (between 6 and 24 months).
Will I be able to see or feel it?
Theoretically it shouldn’t. Only in those cases in which the patient has very thin skin (or skin thinning due to the repetitive use of botulinum toxin in the area) could it become skeletonized (that is, become evident to sight or touch).
Is it a problem if I need an MRI?
No. It does not pose any problem in the face of magnetic forces, although you should inform your doctor due to the interference in the images that it may generate.
What are the chances my body rejects it and I need it removed?
The possibility of rejection is terribly low, since it is a 100% biocompatible material. The incidence of allergy to metals such as titanium is very low (and is normally secondary to other components present in it, such as cobalt, chromium, nickel, copper, iron, etc.). This can be known through a small blood test, which allows validating hypersensitivity to metals.
Is it known to cause infection?
It does not generate infection, although if appropriate measures are not taken during surgery or the surgical bed suffers an infection, it represents a perfect area for bacterial proliferation, making the removal of said material essential if repeated infectious episodes occur.
Has FT changed the type of mesh used in forehead reconstruction?
Yes. Over the years we have seen an improvement in the quality of the material, being more resistant but sufficiently but more ductile. Furthermore, the designs used have been optimized to perfectly adapt to the needs of covering anterior wall or frontal bone defects.
How is it removed, in the event this is necessary?
As it requires unscrewing and removing relatively large fragments, it is necessary to make an incision in a hidden area of the scalp. That is why it is preferred to use the previous approach for this.
Will the forehead bone be weaker than before?
It is said that after a fracture, between 70 and 90% of the previous bone resistance is recovered.
Is it still safe to participate in high impact sports or scuba diving?
Wait at least 4 to 6 months to reactivate impact sports or scuba and always under protection (helmet, chin guard, etc.) until one year old. If in doubt, consult a sports doctor beforehand.







